Vulvodynia: a psychosexual therapist explains.
To talk about sexual pleasure as much as we do at Smile Makers, we also have to talk about sexual pain. Many of us vulva owners live with chronic illnesses such as PCOS, or conditions like vaginismus, that impact our sex lives and wellbeing greatly. The thing is, they are very rarely discussed out in the open, creating yet another sexual taboo. Vulvodynia is one such ‘taboo’. So, we reached out to Alysha Nichol, a Psychosexual & Relationship Therapist, to help break it.
Vulvodynia is thought to affect 5 million women across the UK...
‘I have come across more clients with this condition and it is becoming more regular. It is very much an anxiety-based dysfunction, as are many others. And, it isn’t spoken about enough.
What is vulvodynia?
Vulvodynia can be described as an ongoing, unprovoked pain in the vulva that does not have an overt cause; where other diagnoses have been ruled out by examination and investigation. It may be primary vulvodynia - with no known cause; or secondary - caused by another condition where there is inflammation in the vulva, for example, severe vaginal thrush.
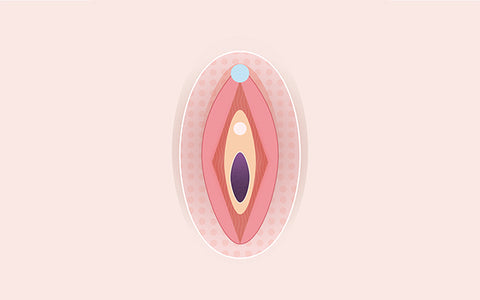
It’s worth noting, as we are often not taught the distinction in our female sex organs, that the vulva and vagina are different. The vulva is the external parts of female genitalia, and the vagina is part of the internal genitalia. To help understand where pain is occurring, mapping the vulva may help!
What are the symptoms of vulvodynia?
This constant or recurrent pain in the vulva can be experienced as:
- Burning
- Stinging
- Throbbing
- Sore feeling
- More unpleasant when sitting down
The pain can be spontaneous or triggered when the vulva is touched, and limited to part of the vulva or more widespread over the genital area, such as the buttocks, upper thigh or anus. For a lot of people, this ongoing pain can cause a lot of discomfort and affect our sexually intimate relationships; be that with ourselves or a partner.
How does this differ to vestibulodyina?
Vestibulodynia (formerly known as vulval vestibulitis) can be used to describe provoked pain arising at the entrance of the vagina, in the area known as the vestibule. This is the space between the labia minora where the openings to the vagina and urethra sit. Pain can be triggered with any pressure, touch or friction and is spontaneous in nature. This type of pain can also be called ‘localised vulvodynia’. Remember, all external female genitalia are part of the vulva.
Diagnosis & causes.
A gynaecologist should be seen for an examination to rule out conditions that can mimic the same symptoms as vulvodynia, before then reaching a diagnosis.
What could be the cause?
Unfortunately, the cause is not known and sometimes the cause can never be found. However, it is thought that vulvodynia may be caused by nerve damage around the vulva area. Nerve endings in the skin on the vulva becomes over-sensitive, sending irregular signals which create a sensitised feeling of pain. This can be from previous surgery, trapped nerves or childbirth. Stress and anxiety can also induce symptoms or make symptoms worse.
Common myths debunked…
- It is not contagious or caused by a sexual transmitted infection.
- It is not hereditary
- It has nothing to do with personal hygiene
- It is not a sign of vulva or vaginal cancer
Can vulvodynia be worse at night?
Vulvodynia can happen spontaneously or be triggered by touch. As mentioned, it can feel unpleasant when sitting down and the same can go for laying down. There are some medications that can be taken to alleviate symptoms that arise prior to or when trying to sleep, following general advice can help deter or alleviate symptoms that may occur in the night. The most important thing is to try to relax and lessen stressors towards bedtime.
Is there a cure or treatment for vulvodynia?
There is no specific treatment or simple cure, but most patients will be helped by of a variety of treatments until the problem subsides. It’s always best to seek advice from your G.P to create a treatment plan. Of course, each doctor has their own method of treatment and every person will respond to treatment differently depending on the type of symptoms experienced. Here’s some general advice and common options to discuss with a doctor...
Managing the everyday:
- Avoid cosmetics with perfume and possible irritants, such as bubble bath or wipes.
- Using a doughnut-shaped cushion if the problem worsens when sitting.
- Navigating stressors in your life which may be contributing to symptoms.
- Tight clothing or underwear more prone to allergies in the genital should be avoided.
- Avoiding sexual intercourse if symptoms are serious or feel severe.
- Communicating with your partner to determine more helpful intimacy techniques and lubricants that are comfortable to both of you.
Topical or over-the-counter treatments:
- 5% Lidocaine local anaesthetic cream, gel or ointment to help numb the area (it is important to note that long-term use of Lidocaine can cause an allergy or resistance.)
- Aqueous cream
- Water-based lubricants
- Coconut oil
- Petroleum jelly
- Capsaicin cream (derivative of chilli pepper)
Prescribed medication:
- Oral medication such as pregabalin, gabapentin and amitriptyline
- Steroid or local anaesthetic injections (vulva injections)
Physical treatment:
- Pelvic floor exercises
- Pelvic floor physiotherapy
Psychological treatment:
- Psychosexual therapy to explore and deal with feelings about the condition. It can also help to discuss feelings and the effects on intimate relationships (G.P referral on NHS or seeking Privately). Please note the NHS waiting list to see a Psychosexual therapist can be up to 6 months. If you decide to consider the private option, it is important to seek a Registered COSRT therapist via the COSRT (College of Sexual and Relationship Therapists) website, www.cosrt.org.uk
- Pain management clinic (G.P referral on NHS)
Surgical treatment:
- Vestibulectomy, a general anaesthetic surgical procedure which removes the sensitive areas of the skin within the vestibule (the area between the lower vagina and just within the vulva). Depending on where the pain is will determine how much and what part of the tissue is to be removed. This treatment is usually considered as a ‘last resort’ but people who have had this treatment have been happy with the results. However, pain or symptoms could still arise after having the procedure.
Sexual pleasure & vulvodynia.
Whilst it’s not recommended to have sexual intercourse when experiencing more serious symptoms, because let’s face it... we want sex to be wholly pleasurable; it doesn’t mean we have to scrap sexual pleasure altogether. Exploring ourselves and communicating with our significant others can help alleviate anxiety around vulvodynia. Rethinking how we get intimate and trying out new techniques to find comfort and pleasure is possible with vulvodynia.
Using sex toys.
The Frencg Lover is a uniquely shaped tongue vibrator that can be used for people suffering with sexual dysfunctions, including vulvodynia. Using the vibration on its lowest setting is extremely subtle, and it can almost mimic a feather. The delicate tongue-shaped tip can be used in different areas of the body, and with lubricant. Of course, each person's experience of this sexual dysfunction is different but this is an excellent choice of vibrator to use for exploring our body’s pleasure, as well as a goal of orgasm through gentle genital stimulation.
A general ‘rule of the thumb’ when it comes to sex toys for vulvodynia is to look for one that has a very low vibration setting or that uses air pressure pulsations.
For more information...
British Society for the Study of Vulval Disease Web: http://www.bssvd.org/
International Society for the Study of Vulvovaginal Disease Web: http://www.issvd.org/
National Vulvodynia Association Web: http://www.nva.org/
References
British Association of Dermatologists Patient Information Leaflet, produced May 2006, review date September 2018 Vulval Pain Society Web: http://www.vulvalpainsociety.org/vps/
NHS https://www.nhs.uk/conditions/vulvodynia/
Written by Alysha Nichol, RegCOSRT Psychosexual & Relationship Therapist PG Dip. Psychosexual & Relationship Therapy BSc (Hons) Psychology www.alyshanichol.com











