Article

Pleasure Tips



Add another to qualify for free delivery.
You’ve qualified for FREE shipping on your order
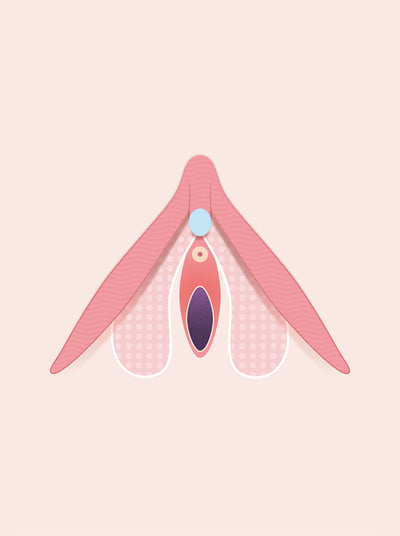
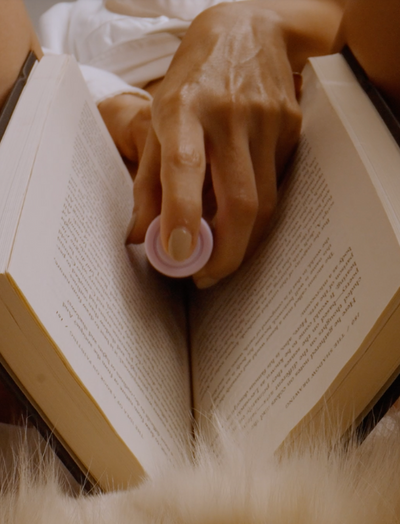
For breast cancer awareness, we want to inspire you to make self-examination part of your normal routine. Our latest series encourages breast self-checks during self-pleasure.






We use cookies to give you the best online experience. Find out more on how we use cookies in our cookie policy.
For more inspo @smilemakerscollection